A Probiotic Solution For Long COVID
Could taking a multi-species probiotic improve symptoms of Long COVID?
We ask this question because the chances are very good that you know someone who has experienced Long COVID.
More than 25 percent of the 134 million Americans who contracted COVID-19 had experienced symptoms of Long COVID, according to Census Bureau data.
Nearly 10 percent of those patients were still struggling with the very same collection of Long COVID symptoms, including brain fog, extreme fatigue, cognitive challenges, insomnia, depression and gastrointestinal problems.
Some of these Long COVID symptoms are connected to the health of your gut and the depletion of beneficial bacteria.
So, is it possible that a probiotic targeted with specific species of bacteria makes a real difference in treating Long COVID symptoms?
The multi-species advantage
Scientists at the Chinese University of Hong Kong addressed this probiotic possibility in a study that tracked the health of 463 patients experiencing Long COVID symptoms for six months.
A group of 232 patients were treated twice daily with a probiotic formulated with three strains of beneficial bacteria from the Bifidobacterium family along with three prebiotic compounds while a second group received a placebo containing starch and a low dose of vitamin C.
(Bifidobacterium longum and Bifidobacterium bifidum are two of the key building block strains of beneficial bacteria contained in EndoMune Advanced Probiotic.)
Patients completed questionnaires that documented 14 symptoms of Long COVID and provided stool samples before the study began and after it ended.
Among those who received probiotics, a majority of them experienced welcome improvements in their Long COVID symptoms in all categories, highlighted by alleviations in memory loss, concentration problems, fatigue and general unwellness, as well as increases in bacterial diversity.
Planning for the future
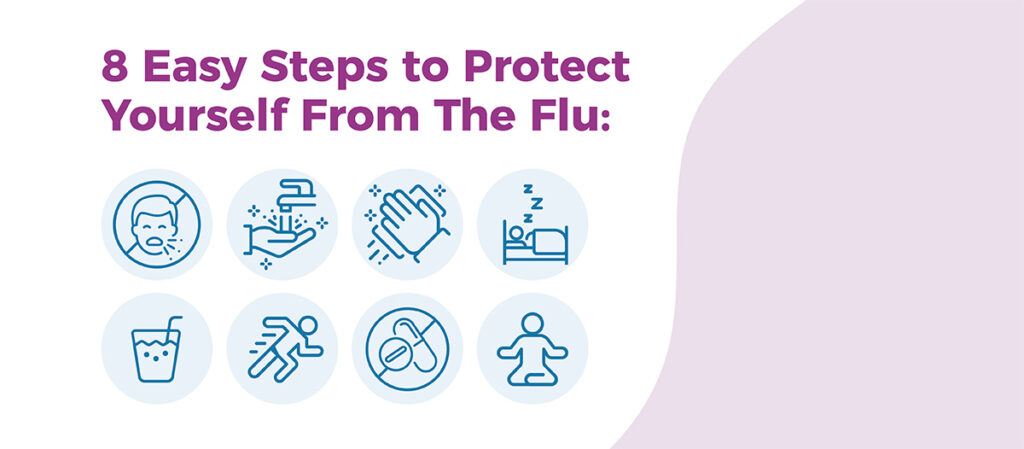
With changes coming in the CDC pipeline that would further loosen COVID isolation recommendations to match those for flu and RSV, it’s more important than ever to protect your immune health.
One of the best things you can do to keep your immune system running as it should be is to protect the diversity of bacteria in your gut which means taking a probiotic, ideally with multiple strains of beneficial bacteria like EndoMune.
By the way, fortifying your immune health is only one of many benefits you’ll get by taking a probiotic. Check out our 5 Reasons Why You Need a Probiotic article to get a handle on the many reasons why taking a multi-strain probiotic like EndoMune is good for many more health reasons.
Resources
A Probiotic Solution For Long COVID Read More »