Treat Diarrhea With Probiotics
Beat Antibiotic-Associated Diarrhea With Probiotics
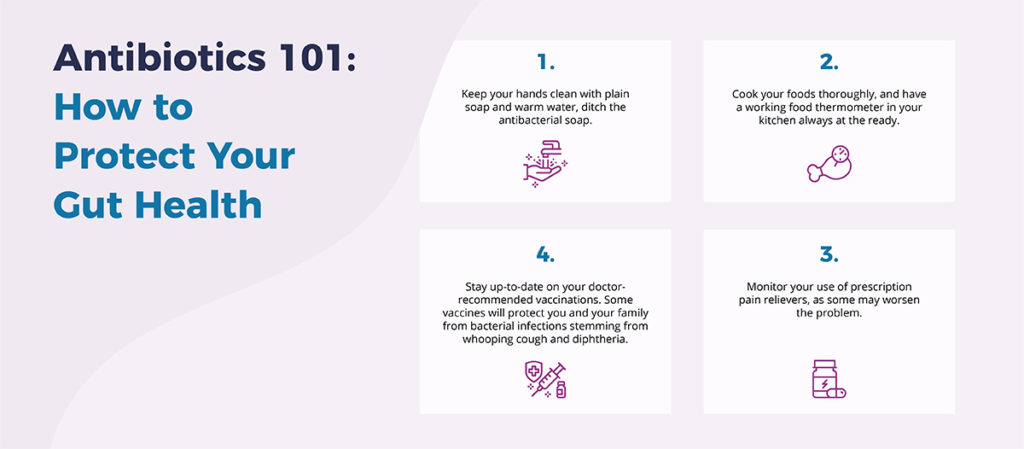
The impact antibiotics have on human health and our gut is one of the most important things modern medicine has learned over the past 20 years.
Antibiotics remain effective tools that treat many problems, but relying on them too often creates additional health complications.
Even when they’re used properly, antibiotics are disruptive to the healthy balance of bacteria in the human gut, spurring antibiotic-associated diarrhea, a very common problem that affects roughly 1 out of every 5 patients.
Fortunately, modern medicine has embraced the important role probiotics play in protecting the healthy balance of bacteria in the human gut, the center of our immune system.
What’s more, probiotics are a safe, effective treatment for antibiotic-associated diarrhea, according to a study recently published in the health journal Nutrients.
The Bifidobacterium Way
Scientists from the University of Maryland and Georgetown University examined the benefits of a proprietary blend of Bifidobacterium lactis on 42 patients who were given amoxicillin-clavulanate, a common antibiotic.
Scientists from the University of Maryland and Georgetown University assigned 38 healthy patients to eat a daily serving of yogurt containing Bifidobacterium lactis for two weeks, along with a standard, week-long regimen of the common antibiotic, amoxicillin-clavulanate.
(Bifidobacterium lactis is one of 10 strains of beneficial bacteria contained in EndoMune Advanced Probiotic and EndoMune Junior Advanced Chewable Probiotic.)
An additional 18 patients were assigned to a control group who ate the daily yogurt minus the probiotic bacteria for two weeks while also taking the antibiotic for a week.
No surprise, patients who took a probiotic had a healthier balance of bacteria in their guts than those assigned to a placebo, but how?
For one, patients assigned the placebo had significantly lesser amounts of the short-chain fatty acid acetate, a metabolite produced by gut bacteria, than those taking a probiotic. In fact, acetate levels among patients in the probiotic group more rapidly returned to normal by day 30.
Additionally, researchers cited the benefits of taking a probiotic the very same day they started their seven-day course of antibiotics.
“Starting the probiotic as early as possible, before the antibiotic symptoms have progressed, may result in a greater opportunity for the probiotic mechanisms to be expressed and may ultimately lead to more beneficial clinical outcomes,” says study co-author Dr. Daniel Merenstein of the Georgetown University School of Medicine.
Follow Your Antibiotic Protocol!
The results of this study were so impressive and positive, the National Institutes of Health plan to fund a follow-up study to determine the best time to take a probiotic.
Luckily, if you follow our blog regularly, you may already have an antibiotic protocol in place, so you already know what to do!
The important thing to remember: Give yourself a two-hour break between a probiotic — ideally one with multiple strains of beneficial bacteria like EndoMune — and an antibiotic to give those beneficial bacteria some extra time to do their work.
Resources
University of Maryland School of Medicine
Treat Diarrhea With Probiotics Read More »