I receive daily emails from a number of sources about new developments in medicine, particularly in the areas of gastroenterology and probiotics.
There are two interesting articles I would like to briefly discuss this month:
- Benefits of Lactobacillus probiotic bacteria against gas-producing E. Coli found in colicky infants(1)
- Probiotics for prevention of antibiotic-associated diarrhea and Clostridium difficile-associated disease in hospitalized adults(3)
Benefits of Probiotic Bacteria for Colicky Infants
The first report details the research that has been underway to determine how probiotics can lessen the problem of “Infantile Colic.” This is a condition in which a healthy baby shows periods of intense, unexplained fussing/crying lasting more than 3 hours a day, for more than 3 days a week over a duration of three or more continuous weeks. Parents have sleepless nights and stressful days trying to calm their baby. The pediatricians used to recommend trying simethicone drops, which works no better than tap water.
The exact cause of infantile colic is unknown, but a number of reports have associated colic to changes in the bacterial balance in a baby’s intestine.
A study published in the journal Pediatrics in 2007(2) reported on the benefits of taking a probiotic. In the study, 83 colicky babies were divided into two groups: 41 were given a Lactobacillus probiotic and 42 babies received simethicone. The results were astounding:
After one week, babies treated with the probiotic had close to 20% less crying time
- By 4 weeks, probiotic treated babies had 74% less crying
- Overall, there was a 95% positive response to the Lactobacillus probiotic drops in colicky infants.
To better understand how probiotics lessen infantile colic, this study was performed to evaluated the interaction between Lactobacillus probiotics and gas-forming coliforms that were isolated from stools of colicky infants. The results showed that several strains of Lactobacillus produced antibiotics against six different species of gas-forming coliforms.
The authors concluded:
- There was a greater presence of of coliform bacteria in colicky infants, and
- Certain Lactobacillus probiotic bacteria can improve colicky symptoms by reducing the ability of coliform bacteria to colonize the gut.
Probiotics for Prevention of Antibiotic-Associated Diarrhea, C. Difficile
This report published in the American Academy of Nurse Practioners reviewed all the relevant studies on probiotic efficacy for preventing diarrhea and colitis due to taking antibiotics.
I have written several newsletters on how antibiotics can upset the healthy balance of the intestinal bacteria, resulting in mild diarrhea or life-threatening clostridia difficile colitis. There are a 100 trillion bacteria in the gastrointestinal tract. Generally, 85% or more are healthy beneficial bacteria that help in digestion and immunity.
Antibiotics prescribed for an infection like sinusitis or bronchitis can destroy the healthy intestinal bacteria and result in problems with diarrhea. A particular bacteria called Clostridia difficile can multiply when the healthy bacteria are destroyed.
C difficile produces toxins that cause a severe colitis. Unfortunately, this bacteria is becoming more common in hospitals and other health care facilities. As a result, the risk of developing colitis and diarrhea has increased. In 2006, it was reported that patients with C difficile colitis stayed in the hospital 3.6 days longer and the additional hospital costs averaged $3,669 per patient day.(4) A conservative estimate of the cost of this disease in the United States was $3.2 billion annually.(5)
This report was to determine if giving probiotics to patients receiving antibiotics would lessen the risk of developing antibiotic-associated diarrhea and C difficile-associated disease.
The meta-analysis found that the administration of probiotics led to a statistically significant relative risk reduction. Compared to patients given a placebo, the patients receiving probiotics had a:
- 44% reduction for antibiotic-associated diarrhea
- 71% reduction for C difficile-associated disease
The authors concluded that administering probiotics concurrently with antibiotics in hospitalized patients could potentially lessen the healthcare spending, morbidity and mortality due to the gastrointestinal complications related to the use of antibiotics.
Articles like these two indicate the amount of research that is going on to determine the health benefits of probiotics. Since I started researching the importance of the healthy intestinal bacteria and probiotics in 2005, the amount of new scientific information published annually is amazing.
(1) Antagonistic effect of Lactobacillus strains against gas-producing coliforms isolated from colicky infants.Savino F, Cordisco L, Tarasco V, Locatelli E, Di Gioia D, Oggero R, Matteuzzi D. BMC Microbiol. 2011 Jun 30;11(1):157.
(2)Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study. Savino F, Pelle E, Palumeri E, Oggero R, Miniero R. Pediatrics. 2007 Jan;119(1):e124-30.
(3) Probiotics for prevention of antibiotic-associated diarrhea and Clostridium difficile-associated disease in hospitalized adults-A meta-analysis.Avadhani A, Miley H.J Am Acad Nurse Pract. 2011 Jun;23(6):269-74
(4) Health care costs and mortality associated with nosocomial diarrhea due to Clostridium difficile.Kyne L, Hamel MB, Polavaram R, Kelly CP. Clin Infect Dis. 2002 Feb 1;34(3):346-53. Epub 2001 Dec 17.
(5) Strategies to prevent clostridium difficile infections in acute care hospitals. Dubberke ER, Gerding DN, Classen D, Arias KM, Podgorny K, Anderson DJ, Burstin H, Calfee DP, Coffin SE, Fraser V, Griffin FA, Gross P, Kaye KS, Klompas M, Lo E, Marschall J, Mermel LA, Nicolle L, Pegues DA, Perl TM, Saint S, Salgado CD, Weinstein RA, Wise R, Yokoe DS. Infect Control Hosp Epidemiol. 2008 Oct;29 Suppl 1:S81-92







 EndoMune Advanced Jr., the only children’s probiotic developed by a board-certified gastroenterologist, has won the much-coveted Parent Tested Parent Approved (PTPA) Winner’s Seal of Approval.
EndoMune Advanced Jr., the only children’s probiotic developed by a board-certified gastroenterologist, has won the much-coveted Parent Tested Parent Approved (PTPA) Winner’s Seal of Approval.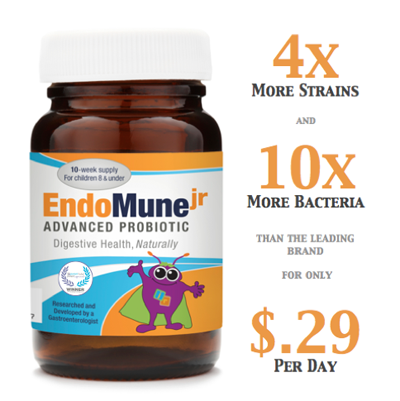 “At PTPA Media, we are proud to play a role in certifying innovative products that families can trust,” says Sharon Vinderine, CEO and founder of PTPA Media Inc. “When consumers search for our Seal of Approval on product packaging and web sites, they are essentially searching for validation from their peers. Their peers will have objectively tested and approved these products based on their performance in a real life environment. That type of resource for families is priceless.”
“At PTPA Media, we are proud to play a role in certifying innovative products that families can trust,” says Sharon Vinderine, CEO and founder of PTPA Media Inc. “When consumers search for our Seal of Approval on product packaging and web sites, they are essentially searching for validation from their peers. Their peers will have objectively tested and approved these products based on their performance in a real life environment. That type of resource for families is priceless.”