IBS + Fibromyalgia + Chronic Fatigue Syndrome
Summary: The gut-brain link between irritable bowel syndrome (IBS), fibromyalgia and chronic fatigue syndrome (CFS) is very real.
Several months ago, we discussed the genuine link between irritable bowel syndrome (IBS) and disruptions in the gut-brain axis.
It’s hard to deny that connection, given that IBS patients experienced greater symptoms of depression and anxiety at rates more than double the norm compared to those without IBS.
Apparently, this same research team from the University of Missouri was just getting started in finding connections with IBS…
The painful link
A second look at data collected from more than 1.2 million IBS patients at 4,000 American hospitals yielded new connections with fibromyalgia, a condition punctuated by widespread and intense musculoskeletal pain, fatigue and cognitive problems, as well as chronic fatigue syndrome (CFS).
IBS patients were five times more likely to experience symptoms of fibromyalgia than those who weren’t dealing with IBS, according to the study appearing in the medical journal Biomedicines. Also, CFS was more prevalent among IBS patients, but not at as high a rate as fibromyalgia.
One interesting quirk in this analysis sheds light on younger people experiencing more gut-related problems than ever before: IBS patients with fibromyalgia or CFS were more likely to be younger compared than others dealing solely with IBS.
Also, the ever-present problems we face with the epidemic of obesity along with hypertension elevated the risks that IBS patients would face CFS or fibromyalgia too.
The why
When asked how fibromyalgia or chronic fatigue syndrome could “piggyback” with IBS to create new and painful challenges, scientists pointed to two very familiar culprits that create gut health problems:
- Antibiotic use leads to bacterial imbalances in a patient’s microbiome.
- Breakdowns in the gut wall allow waste products, toxic substances and other nasties to seep through the intestinal barrier and into your bloodstream, a condition better known as leaky gut.
Fortunately, the same non-drug solution for treating IBS — probiotics — is also a solution that has garnered some success in treating patients with fibromyalgia and CFS, according to a previous report. But not any probiotic will do.
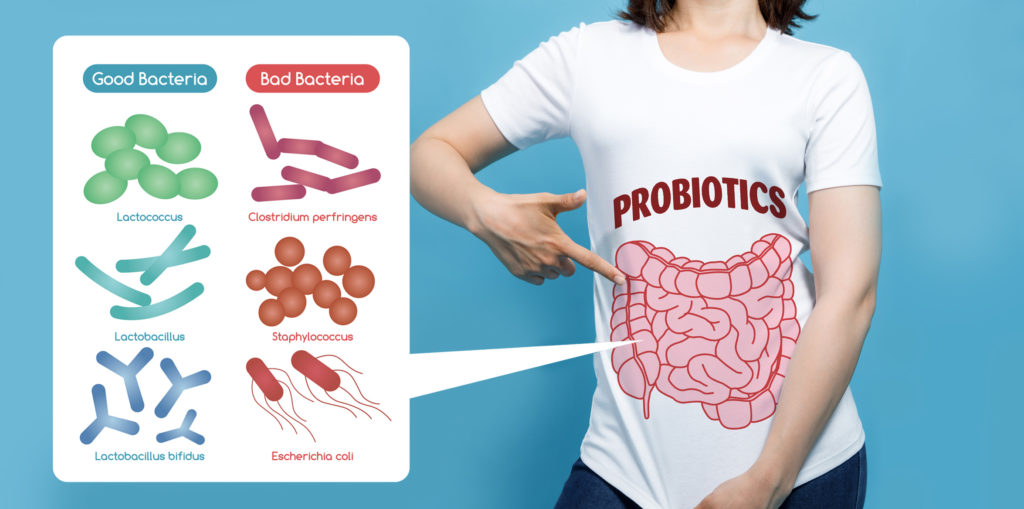
If you really want to protect and improve the health of your gut, you’ll need a probiotic featuring multiple strains of beneficial bacteria that support the healthy microbial diversity of your gut.
Any probiotic you consider should also contain a prebiotic, the unsung heroes of gut health made of carbohydrates and non-digestible plant fibers that feed the good bacteria in your gut.
You can achieve both of your gut-healthy goals with EndoMune Advanced Probiotic, formulated with 10 strains of beneficial bacteria from Bifidobacterium and Lactobacillus families, plus the proven probiotic FOS.
Resources
IBS + Fibromyalgia + Chronic Fatigue Syndrome Read More »