Digest This
Click on the topics below to learn how probiotics can improve your digestive health, naturally.
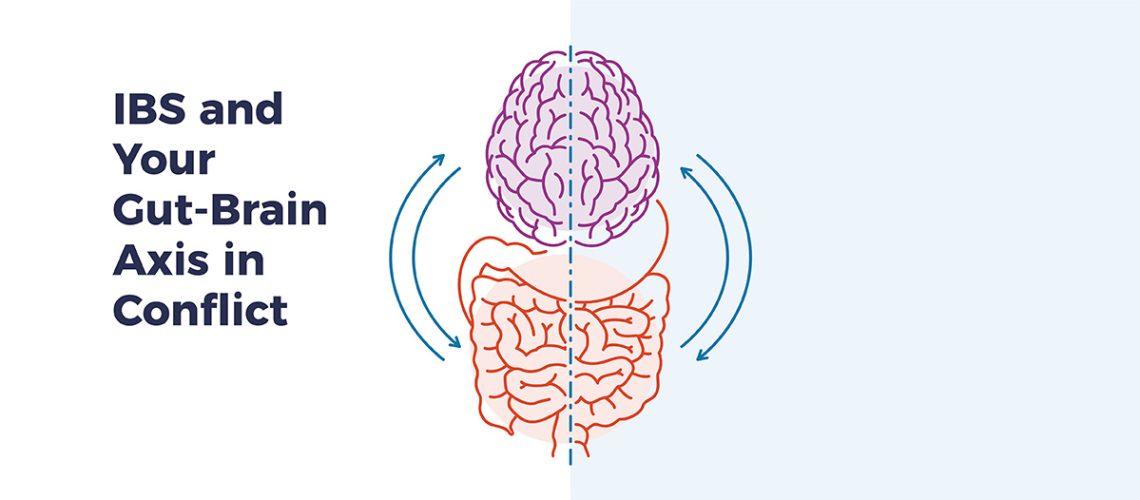
IBS and Your Gut-Brain Axis in Conflict
- @drHoberman
- Mental Health
IBS and Your Gut-Brain Axis in Conflict
A good argument can be made for irritable bowel syndrome (IBS) being not only the most common condition gastroenterologists diagnose — it affects an estimated 15 percent of all Americans — but one of the most challenging ones too.
But familiarity doesn’t guarantee clarity, considering IBS comes in three different subtypes: IBS-D (diarrhea), IBS-C (constipation) and IBS-A (a mix of diarrhea and constipation).
An aspect of IBS that’s rarely explored: its potential impact on your gut-brain axis, the connection that links your brain, intestines and emotions.
So, it should come as no surprise that mental health issues are much more prevalent among IBS patients than those who aren’t, based on an analysis of data conducted by researchers from the University of Missouri.
Mental Health Challenges and IBS
Scientists collected mental health data on more than 1.2 million IBS patients hospitalized in 4,000 U.S. hospitals over a three-year period from a national database, according to the study appearing in the Irish Journal of Medical Science.
More than 800,000 IBS patients in a hospital setting experienced symptoms of anxiety (38 percent overall) or depression (27 percent overall) at rates more than double the norm compared to people without IBS.
Overall, the prevalence of those problems plus bipolar disorder, suicidal attempts/ideation and eating disorders was significantly higher than the general adult population.
This is where the gut-brain axis comes into play, says Dr. Zahid Ijaz Tarar, lead researcher and assistant professor of clinical medicine at the University of Missouri. “Medical professionals need to treat both ends of the axis.”
“I frequently tell my patients who have IBS that, if they have any type of psychologic stress, it will get expressed in some form or another,” says Yezaz Ghouri, senior author and assistant professor of clinical medicine and gastroenterology at the University of Missouri.
Given that at least 90 percent serotonin your body produces is generated in the gut and specific bacteria play key roles in producing it, disruptions from IBS or other gut health issues do matter.
Solutions For Treating IBS and Gut-Brain Axis
If you suffer from IBS and have emotional challenges because your gut-brain axis is out of balance, plenty of good options are available that help out on both fronts.
For example, cleaning up your diet, devoting some time each week to exercise and paying attention to your sleep can do a lot of good.
If managing your stress becomes a challenge, your physician may want to prescribe an antidepressant drug like a selective serotonin reuptake inhibitor (SSRI) like fluvoxamine or an older tricyclic drug like amitriptyline.
You’ll also want to consider taking a probiotic, a proven and effective non-drug solution that helps your gut and brain at the same time. But not just any probiotic will do…
A probiotic formulated with proven strains from the Bifidobacterium and Lactobacillus families, like those contained in EndoMune Advanced Probiotic, can go a long way toward relieving your IBS and rebalancing your gut-brain axis safely and effectively.
Resources
There Is An Endomune Probiotic For Every Lifestyle
-
EndoMune Metabolic Rescue
$44.95 -
EndoMune Advanced Probiotic
$42.95 -
EndoMune Companion Pack
$112.93